As part of Diabetes week, one of our Lead Analysts, Tom, discusses his family’s personal experience with type 1 diabetes, and the blood glucose technology available to support management of type 1 diabetes.
My family’s introduction to diabetes began in 2015. I was deep into a difficult biochemistry module in my second year at uni. My brother (aged 8) had been unwell for a few weeks – all he could stomach was water, and sugary custard. He went to the GP on multiple occasions, but his illness was considered an infection – Mum was certain it was something more. After several visits, a finger prick test was done, and he was blue-lighted to hospital. Typical blood glucose levels for a healthy individual are up to 7.8mmol/L after eating – my brother’s was. 34mmol/L.
My brother was swiftly diagnosed with type 1 diabetes. I packed a bag and hopped on the train to be with my family. I hadn’t eaten properly that day (student diet) and took a wrong turn trying to get to East Surrey hospital. After traipsing across a few fields with a suitcase, I arrived at East Surrey exhausted and nearly passed out – the last thing the nurses and my family needed.
The first few days were scary, but you quickly become the experts. I vividly remember my mum’s first attempt at giving my brother an insulin injection. How hard are you supposed to press? Mum wound up her arm and came down like pickaxe into my brother’s leg… the nurses winced at the amount of force applied. The next challenge was convincing an eight-year-old to voluntarily draw blood from his own fingers. We spent days and days fingerpricking each other’s toes before getting brave enough to move to fingers. With my health economics hat on, we must have spent a fortune on lancets, but it was all worth it.
My brother is 17 now. He’s taller than me (and it hurts to admit it), he’s learning to drive (with a few additional DVLA hurdles), and he’s about to be my best man. Everyday has its challenges for him, but it has been made much easier with the improvement made in medical technology, and we are so thankful for it.
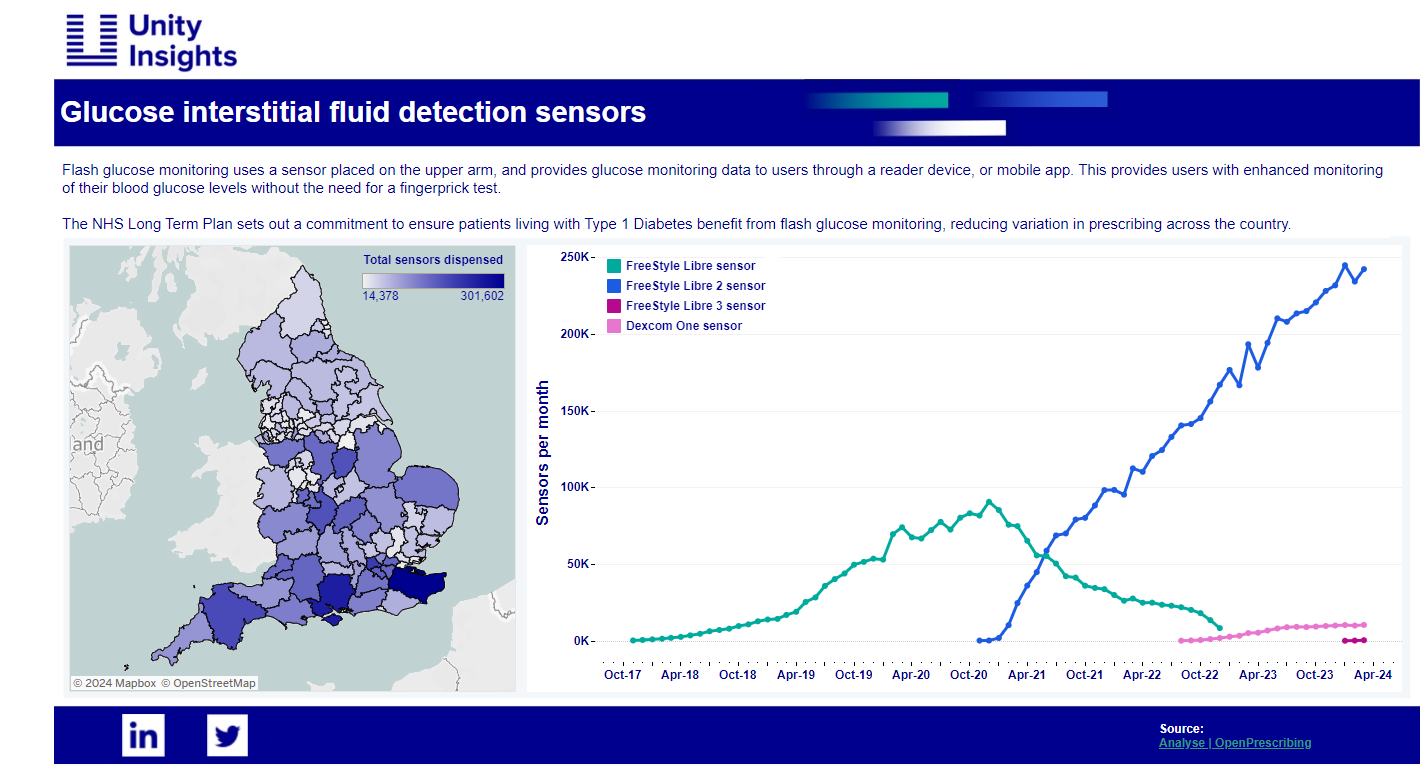
The rise of the machines supporting people living with T1D manage their blood glucose levels has been an exciting space in recent years, with new technologies advancing beyond fingerprick tests, and policy changes making these new technologies more easily accessible to people. This all started in November 2017 with the introduction of Freestyle Libre on the NHS drug tariff, providing blood glucose levels without having to conduct a fingerprick test. Instead, users would have a sensor placed on the back of their arm (other locations available), and would pass a reader over it which reports their blood glucose level. Theresa May was one of the first public figures to be sporting one of these sensors, if you’ve ever wondered what she was wearing on the back of her arm.
In 2022, Dexcom ONE continuous glucose monitoring became available, actively sending blood glucose readings to a meter, smartphone and smart watches without having to pass a reader over a sensor.
In recent months, hybrid-closed loop systems, also known as artificial pancreases, have been rolled out across the NHS. The system combines glucose monitoring systems with insulin pumps to automatically detect a person’s blood glucose levels, and administers the appropriate dosage of insulin. The nearest we have got to hands-free T1D. My brother hasn’t taken this step yet – but during that difficult biochemistry module – we reviewed a few very early papers from America looking into this sort of technology and it just felt so far away, I cannot believe we are here now.
I have a real passion for this area, and at Unity Insights we are interested in all elements of support and care for type 1 and type 2 diabetes – whether that be innovative technology for managing blood glucose levels, novel ideas for delivering structured education and lifestyle changes, or mental health support.
If you have a new idea or technology, and need support in growing its evidence base, please come and have a chat 😊
Get in touch: enquiries@unityinsights.co.uk
