Head and neck cancer (HNC) is a rare type of cancer that presents with common symptoms. This may lead to a delay in referrals for suspected HNC patients from primary care. Amidst heightened staff pressures and increasing patient referral volumes, improving the efficiency of suspected cancer pathways is crucial to achieve the 28-day Faster Diagnosis Standard (FDS) target, and the goals set out by the NHS Long Term Plan.
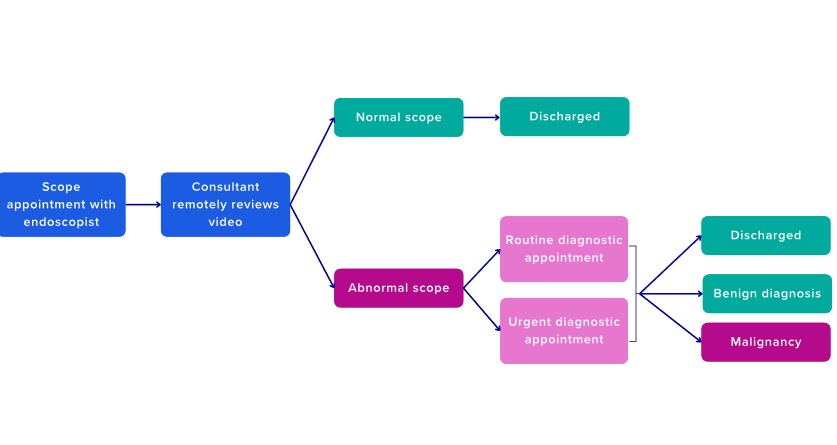
Implementing the telescopic referral pathway may facilitate rapid HNC diagnosis for high-risk patients. Through diverting low-risk patients through an alternative pathway to capture high-definition endoscopic videos, specialist HNC consultants can remotely review each suspected HNC patient more efficiently. By proposing a bespoke solution that is accessible and portable, the telescopic technology may facilitate a more streamlined HNC referral pathway through the involvement of allied healthcare professionals in endoscopy procedures.
The Small Business Research Initiative (SBRI) bid for telescopic referrals was successful and awarded funding as part of the SBRI NHS Cancer Programme Innovation Open Call 1 for the competition in Spring 2021. Unity Insights provided support through two methods of evaluation. Supported by Wessex Cancer Alliance, the current rollout at University Hospitals of North Midlands NHS Trust (UHNM), and a pilot at Dorset County Hospital NHS Foundation Trust (DCHFT) were retrospectively evaluated where possible to assess the implementation and potential prospective impact of the pathway. A different approach of utilising the telescopic technology was adopted at each site. Only the implementation of the telescopic referral pathway at Royal Stoke University Hospital (RSUH) was modelled for the purposes of the health economic methodology; however, quantitative, and qualitative analysis was conducted at both RSUH and Dorset County Hospital (DCH).
Quantitative analysis at RSUH identified that low-risk patients who were given a telescopic referral had an average of 28.6 days to diagnosis (n = 625; January 2021 – December 2022). At RSUH, one consultant continues to use the traditional HNC pathway, and two consultants use the telescopic referral pathway. For a mixture of low and high-risk patient at the same site, an average of 32 days to diagnosis was recorded (n = 367; July 2023 – September 2023); however, different data collection periods and patient groups limit direct comparability. At DCH, the average days to diagnosis using the telescopic technology without implementing the telescopic referral pathway resulted in an average of 38.8 days to diagnosis.
Qualitative analysis at RSUH and DCH suggested that staff and patients that utilised the telescopic technology reported a positive experience.
During interviews, clinical staff reported:
- Ability to see more patients due to quicker appointments and better prioritisation of patients.
- Satisfaction regarding the ease of use and portability of the technology, with equipment and connectivity issues rarely occurring.
- Improved communication and collaboration among the staff.
Patient survey responses recorded at both RSUH and DCH suggested that telescopic technology facilitated quicker access to appointments and increased transparency, indicating that patients regard the telescopic technology and referral pathway as an acceptable and credible solution.
Cost-benefit analysis based on implementation of the telescopic referral pathway at RSUH was modelled across three distinct scenarios: the RSUH site (scenario 1), the West Midlands region (scenario 2), and across England (scenario 3). The following benefits were modelled:
- Reduction in face-to-face (F2F) consultant appointments
- Reduction in unnecessary diagnostic procedures
- Eliminated need for additional equipment and maintenance (modelled for scenario 2 and 3 only)
In scenario 3, the total modelled benefits and costs come to £5.6m and £12.9m, respectively. For this national extrapolation, the benefit cost ratio (BCR) indicates an improved return on investment of £0.4 for every £1 spent. Notably, for scenario 3, the BCR increased from 0.2 in Year 1 to 0.4 for Year 2, and 0.6 for Years 3 to 5, and 0.9 at Year 10, showing a long-term potential for near full pay back.
To breakeven in scenario 1, approximately 2,012 low-risk patients per year would be required to attend a telescopic referral pathway appointment. For scenario 3, the breakeven point was approximately 1,877 patients per site annually. Therefore, if more patients were seen on the telescopic referral pathway at each site across a time horizon extended beyond five years, a better return could be achieved.
Alternatively, if a site has needed to run additional clinics to address increased HNC referral volumes, implementing the telescopic referral pathway may help to yield greater potential benefits than are included in the full health economic model. An additional modelled scenario (scenario 4) indicated that at RSUH, the potential benefit of avoiding additional clinics over the course of five years may enable the BCR to achieve improved return on investment of £0.7 for every £1 spent from Year 2 onwards.
The following key recommendations were made to improve the cost-effectiveness and quality of service.
- Centralised sites: It is expected that suspected HNC referral volumes will increase over time, but this will eventually plateau. Based on the sensitivity analysis results, centralised secondary care sites should be investigated as a possible way to receive greater patient volumes from across wider geographical regions to make the most of the upfront cost of the telescopic technology.
- Community-based sites: The use of the telescopic referral pathway in community-based sites may not only improve access to patients who may have otherwise faced health inequalities regarding cancer diagnosis, but may also facilitate the upskilling of Band 4 nurses or community health workers to conduct scope appointments.
- Data collection: To obtain better insights and evaluate the economic value of the telescopic referral pathway more accurately (for example, measure some of the currently unmodelled benefits) requires the collection of more granular data points. Further, by recording whether a patient was re-referred by a GP within the following six-month period, the efficacy of the telescopic referral pathway may be demonstrated, based on whether comparatively less cancers are missed using this technology compared to the traditional pathway.
Conclusion
The telescopic referral pathway leads to positive outcomes for both patients and staff, specifically by prioritising high-risk patients, providing faster diagnosis to patients on the suspected HNC pathway, and improving the efficiency of limited specialist HNC consultant resource. By comparing RSUH and DCH, it is evident that the telescopic technology is best suited when used as part of the telescopic referral pathway to achieve improved efficiency for suspected HNC patients. To achieve 28-day FDS, and ultimately help to achieve the goals of the NHS Long Term Plan, it is important to identify low-risk patients early and divert these patients to an alternative telescopic referral pathway, allowing high-risk patients to be prioritised, to ensure that all patients are diagnosed more promptly.
Get in touch with us
- Phone
- Email enquiries@unityinsights.co.uk
