Barrett’s oesophagus occurs when the inner lining at the lower end of the oesophagus is damaged due to acid reflux and can develop into oesophageal cancer. Unity Insights were commissioned to evaluate the impact of a minimally invasive, non-endoscopic diagnostic test for the detection of Barrett’s oesophagus and early oesophageal cancer for individuals living with chronic reflux.
The two main patient cohorts examined were:
- Proactive case finding: Patients living with chronic reflux who were at risk of oesophageal cancer were invited to take a non-endoscopic diagnostic test in Primary Care
- Barrett’s surveillance: Patients already diagnosed with Barrett’s oesophagus and requiring surveillance who were at risk of oesophageal cancer were offered the test in replace of an endoscopy.
Clinical impact of the non-endoscopic diagnostic test
Compared to a previous clinical trial, the findings were similar, suggesting replicability of results in a primary care environment:
- A similar number of tests were completed (current innovation: n = 1,673; clinical trial: n = 1,654)
- A similar adequacy rate was yielded (current innovation = 88%; clinical trial = 88%)
- A similar rate of cancer diagnoses was yielded (current innovation = 0.16%; clinical trial = 0.24%)
On average the pathway took 32.5 days for a triaged patient to obtain their results, much faster than if they were to seek treatment once their symptoms had worsened.
The use of the non-endoscopic diagnostic test to assist in early detection of Barrett’s oesophagus and oesophageal cancer had a positive impact on patient outcomes by enabling earlier diagnosis and treatment, which facilitated early identification of individuals who might not have otherwise sought care.
Economic viability of using the non-endoscopic diagnostic test
The non-endoscopic diagnostic test demonstrated a positive return on investment for the health and social care system across one to ten years, driven by improved quality of life and life expectancy (86% of the total benefit). This evidenced a valid economic case for using the test as a proactive case finding tool.
Sustainability of the non-endoscopic diagnostic test across system levels
Figure 2 shows a decrease in the additional endoscopies required over time with endoscopies saved increasing from year 5 onwards. This highlights that the non-endoscopic diagnostic test is a useful long-term approach due to the endoscopies saved over time, however, does generate endoscopies in the short-term. This demand can be mitigated by extending utilisation of the non-endoscopic diagnostic test to support Barrett’s surveillance, or triaging cases already within the endoscopy waiting list (for example, reflux patients).
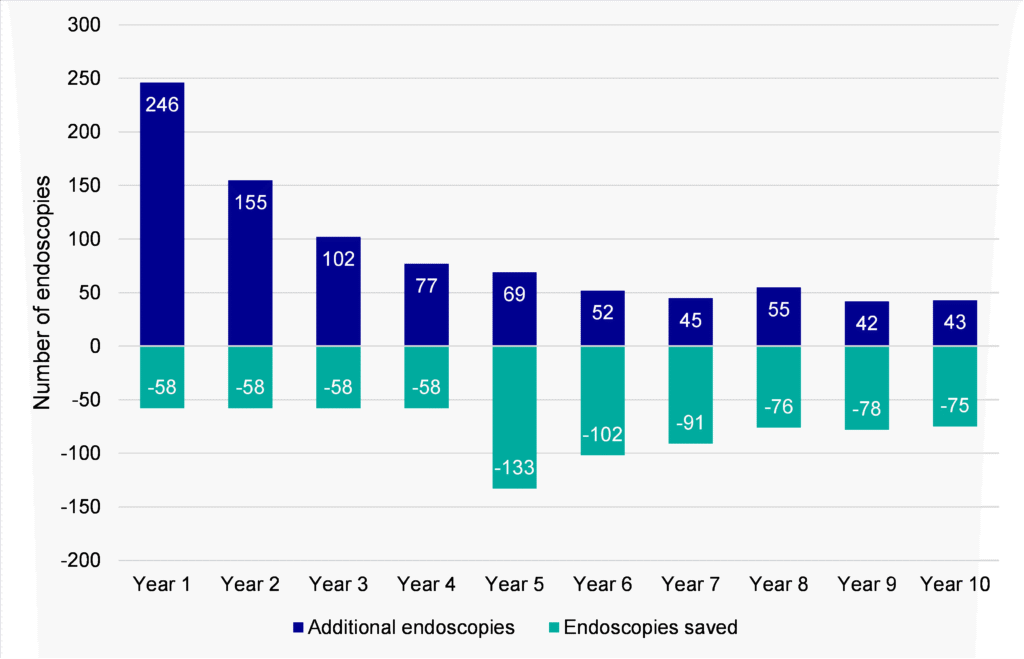
A phased approach to proactive case-finding, managing the number of invites sent per year, may help ensure endoscopic services are not overwhelmed.
Patient and clinician acceptability
of proactive case finding patients had a positive experience throughout the pathway
of Barrett’s surveillance patients had a positive experience throughout the pathway
of staff thought the non-endoscopic test was a reliable and acceptable method for the detection of oesophageal cancer and Barrett’s oesophagus
Over half of staff (53%) considered the triaging process to be efficient. Despite this, in one Cancer Alliance, longer triage times (23.7 days, compared to an average of 9.3 days for all Cancer Alliances combined) drove lower staff efficiency scores (38% considered the triaging process to be efficient).
The pathway stage with the lowest proportion of ‘good’ or ‘very good’ ratings was the procedure itself (proactive case finding = 77%; Barrett’s surveillance = 78%), which was reported to be uncomfortable in some cases.
Overall, patients had a positive experience throughout the pathway. Staff were satisfied with the non-endoscopic diagnostic test pathway overall and considered this a reliable and acceptable method for the detection of oesophageal cancer and Barrett’s oesophagus. Staff were less satisfied with the triaging process compared to other stages of the pathway.
Acceptability and scalability of the non-endoscopic diagnostic test in the reflux pathway
Most staff (74%) agreed that there were enough resources available to support ongoing delivery of the non-endoscopic test across all Cancer Alliances
There were approximately four non-endoscopic tests per courier trip. Further optimisation of clinic booking systems may result in a larger number of non-endoscopic tests in each trip, which could lower the overall cost of testing and make large-scale testing more feasible
Most staff considered the non-endoscopic diagnostic test to be an acceptable diagnostic tool across all Cancer Alliances.
Recommendations
To improve triaging efficiency, streamline the SOP through regular reviews, audits, and continuous improvements to meet changing demands
To reduce the cost of the non-endoscopic tests and improve scalability, complete more non-endoscopic tests per clinic
To upskill staff, create a best-practice forum on FutureNHS, allowing staff members in training to seek guidance from more experienced staff
To enable greater visibility of end-to-end patient journeys, improve data capture within the non-endoscopic test pathway
Conclusion
In a real-world setting, the non-endoscopic diagnostic test yielded positive patient outcomes including early diagnosis of two oesophageal cancers, one gastric cancer, and 73 cases of Barrett’s oesophagus. This enabled earlier diagnosis and treatment, which facilitated early identification of individuals who might not have otherwise sought care.
The non-endoscopic diagnostic test yielded a positive return on investment, with a net present value of £964k over 10 years and a benefit-cost ratio of 1.2. To improve economic value further, optimising clinics and streamlining pathway processes is recommended.
Staff and patients found the non-endoscopic diagnostic test to be an appropriate tool for the early detection of Barrett’s oesophagus and oesophageal cancer, with both cohorts noting the importance of early detection.
Overall, the non-endoscopic diagnostic test shows promise as a screening tool for the early detection of Barrett’s oesophagus and oesophageal cancer. Finding ways to streamline the pathway would further improve the economic case for the non-endoscopic diagnostic test and make larger-scale testing more feasible.
Caveats
Missing data meant that assumptions based on literature and clinical input had to be made in some cases, impacting the quantitative, health economic, and system dynamic modelling analysis.
Extrapolations were made within the data to estimate the impact of the non-endoscopic diagnostic pathway; hence findings should be viewed with consideration.
Our insights
Evaluation design and support for Surrey Mental Health and Wellbeing initiatives
Developing evaluation strategies for a wide range of mental health and wellbeing projects in Surrey
A cost-benefit analysis and high-level carbon impact analysis of the UniWee
Unity Insights conducted a cost-benefit analysis and high-level carbon impact analysis of the UniWee.
Understanding the impact of a non-endoscopic diagnostic test pathway upon cancer pathways using System Dynamics Modelling
The use of system dynamics modelling within a mixed-methods evaluation of a non-endoscopic diagnostic test pathway for B
Mixed methods evaluation of The RealBirth Workshop at Epsom and St Helier Hospitals
An SBRI-funded pilot of The RealBirth Workshop at Epsom and St Helier Hospitals between January 2024 and December 2024.
A mixed-methods evaluation of Clera, a web application designed to support communication between clinicians, patients, and families.
Mixed-methods evaluation of Clera, an application that provides care updates.
Independent evaluation partners in the REVISE HCC project
Our work as independent evaluators of navify® GAAD
Anya: An evaluation of the digital health app for women’s health
Anya: An evaluation of the digital health app for women’s health
A mixed-methods evaluation of a Strategic Optimisation Service of the domiciliary care workforce
A mixed-methods optimisation evauation
Health inequalities advisory support at Kent and Medway NHS and Social Care Partnership Trust (KMPT)
Advisory support on health inequalities for Kent and Medway Partnership Trust
Mixed-methods evaluation of a digital health information and remote monitoring app for heart failure
Mixed-methods evaluation of a heart failure remote monitoring app
An analysis of medicines optimisation solutions
Health economic analysis of a medicines optimisation solution
In Our Own Words: Logic model workshops
Co-designing a logic model to support Youth Researchers in Surrey
