Context of our work
Unity Insights, working in collaboration with the Health Innovation Network Polypharmacy central team and regional Health Innovation Networks, developed a suite of case studies incorporating NHS Business Services Authority (NHSBSA) polypharmacy comparator data, and academic literature, to estimate health outcomes and potential health economic savings across five different polypharmacy indicators and ICB regions.
The Health Innovation Network developed and led the national Polypharmacy Programme between 2021 and 2025, aimed at addressing the challenges associated with the use of multiple medications, particularly in older adults and those with multiple long-term conditions. The Polypharmacy Programme has been executed via its three pillars, and included the establishment of regional and local learning systems:
- Pillar 1 – Population Health Management: Population health management utilising the NHSBSA ‘polypharmacy prescribing comparators’ dataset to highlight variation in polypharmacy prescribing at GP Practice, PCN and ICB level and identify patients for prioritisation for a Structured Medication Review (SMR).
- Pillar 2 – Education and Training: Delivering the Polypharmacy Action Learning Sets (ALS) to upskill the primary care workforce to be more confident about stopping unnecessary medicines.
- Pillar 3 – Public Behaviour Change: Deploying a selection of public-facing campaigns to support patients to understand and get the most from their Structured Medication Review.
How we evidenced the impact of the polypharmacy programme
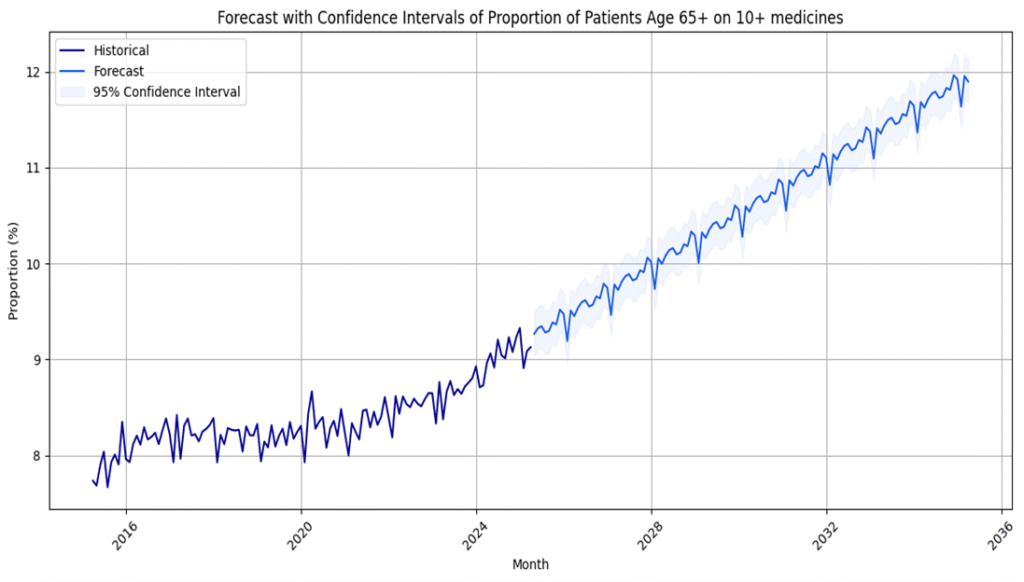
Unity Insights were able to access NHSBSA polypharmacy comparator data hosted on the EPACT2 data system. Using this data, Unity Insights articulated the difference in prescribing rates during the implementation period of the Polypharmacy Programme compared to the baseline period, and converted this to a number of patients that had benefitted.
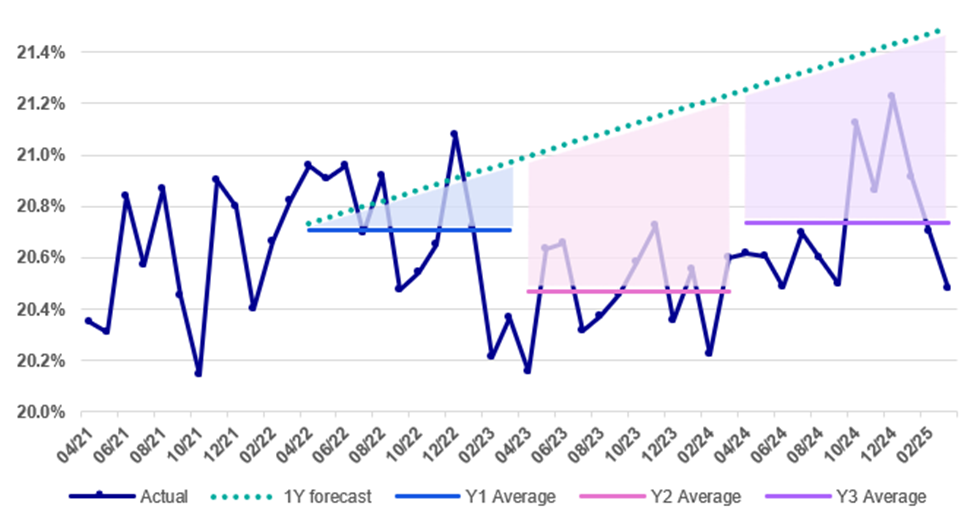
Each NHSBSA Polypharmacy comparator is synonymous with potential untoward outcomes should a patient be on an excessive number of medications – for example, patients on multiple anticoagulants and antiplatelets have a substantially increased risk of experiencing a major bleed requiring hospitalisation. Unity Insights conducted a thorough literature review for each of the NHSBSA Polypharmacy comparators to estimate the increased risk of hospital resource utilisation for patients above the comparator thresholds, and attributed economic values to each incident.
Additionally, NHSBSA supported through the provision of analysis identifying the monetary value of medicines prescribed for patients previously above and below each NHSBSA Polypharmacy comparator.
The final report also estimates the potential cost of the Polypharmacy Programme from the perspective of staff time required to attend the training course.
The results
Across the 5 case studies, Unity Insights were able to estimate benefits to the healthcare system totalling £20.4k in reduction in healthcare resource utilisation, and a further £76k in cash-releasing savings via a reduction in medicines costs. In an additional opportunity analysis, Unity Insights forecasted the potential savings had the whole of England delivered improvements equal to each of the ICB case studies. In these scenarios, an opportunity of £280k was estimated in reduced healthcare resource utilisation, and a further £880k in reduced in medicines cost.
The full report can be found on the Health Innovation Network’s Polypharmacy shared learning platform: Polypharmacy – The Health Innovation Network
Some more of our insights:
Understanding the impact of Magic Notes through validating evaluation findings
The impact of Magic Notes at Kent County Council through validating an evaluation.
Evidencing economic benefits to reducing polypharmacy
A quantitative evaluation of the Health Innovation Network’s polypharmacy programme
Unity Insights’ Partnership with the Health Innovation Network
An overview of Unity Insights’ longstanding partnership and collaboration with the Health Innovation Network
